Examples and Case Studies of Climate-SRHR MEL
Case Study 01:
Addressing Heat Risks to Pregnancy at Maternity Hospitals
Introduction
Extreme heat events are becoming increasingly frequent due to climate change - with adverse impacts on maternal health. Pregnant women increasingly face risks of heat stress, dehydration, pre-eclampsia, preterm birth, low birthweight, spontaneous abortion/miscarriage, stillbirth, and even death as a result of exposure to extreme heat (Lakhani et al. 2024, Li-Maloney et al. 2025, Arunda et al. 2024).
When a local non-profit SRHR organization realized that maternity hospitals in their region lacked the capacity and infrastructure to manage extreme heat risks, they decided to develop a three-year project to address these risks. They plan to submit the project proposal to a funder who has recently put out a RFP for climate-responsive health proposals.
Developing the project concept and theory of change
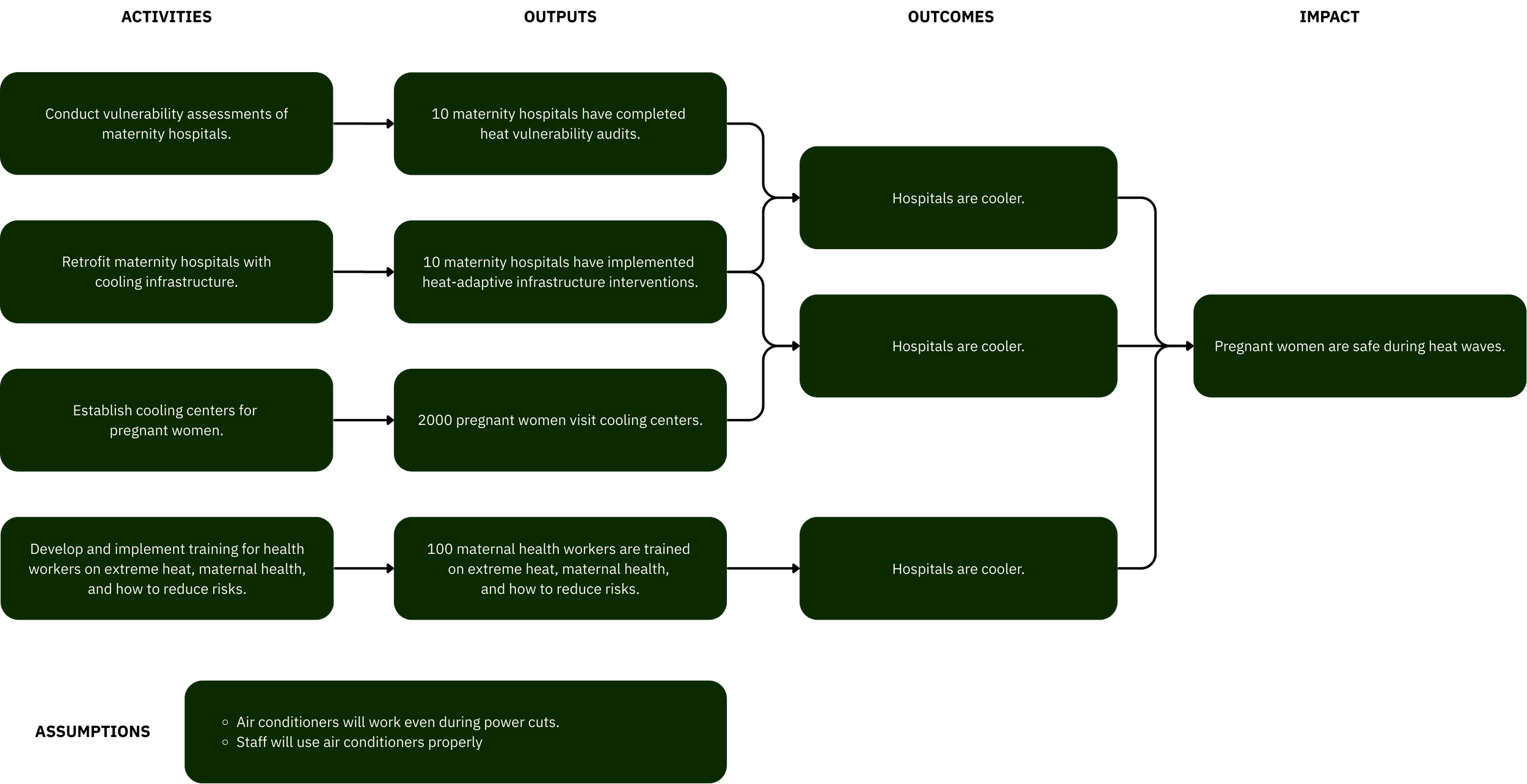
The team knows that the climate hazard they want to focus on is “extreme heat,” and the SRHR domain they want to focus on is “maternal health.” Their first theory of change focused on installing cooling technologies at health facilities and training staff:
They share this initial theory of change framework with an advisory board member. The advisory board member notes that the theory of change is too simple and general. It has some inconsistencies, which make it confusing.
The team then returned to the literature to read more about the mechanisms by which extreme heat exposure impacts pregnant women. They speak with maternity hospital staff and community members in regions that would benefit from the program to learn more about their needs. Based on this evidence, they determine that if pregnant women are less exposed to extreme heat and health facilities and their staff are better prepared for extreme heat risks to pregnancy, then pregnancy and neonatal outcomes will improve at heat-affected maternity hospitals.
They decide on a project with three objectives:
Improve the adaptiveness of maternity hospitals to extreme heat
Reduce pregnant women’s exposure to extreme heat
Increase the knowledge and capacity of maternity hospital staff about extreme heat risks to maternal health and strategies for addressing those risks.
Their target population includes pregnant women visiting maternity hospitals and maternity hospital staff.
Their key interventions include:
Installing heat-adaptive infrastructure at maternity facilities, such as white roofs, solar-powered air conditioning, insulation, ventilation, fans, moving maternity wards to lower levels, etc.
Establishing cooling centers for pregnant women where they can cool off during hot days or electricity blackouts, as well as receive information about heat and pregnancy,
Training maternity hospital staff on heat risks during pregnancy and how they can reduce those risks
Remember, this is one project! Other projects might include different activities, such as heat warning systems, improved heat and maternal health data collection systems, community outreach campaigns, policy advocacy campaigns, heat insurance, home or workplace infrastructure adaptations, etc.
Based on this updated approach, they develop a revised theory of change diagram:
Now that they have a clear sense of their project’s activities and objectives, they’re ready to begin choosing indicators.

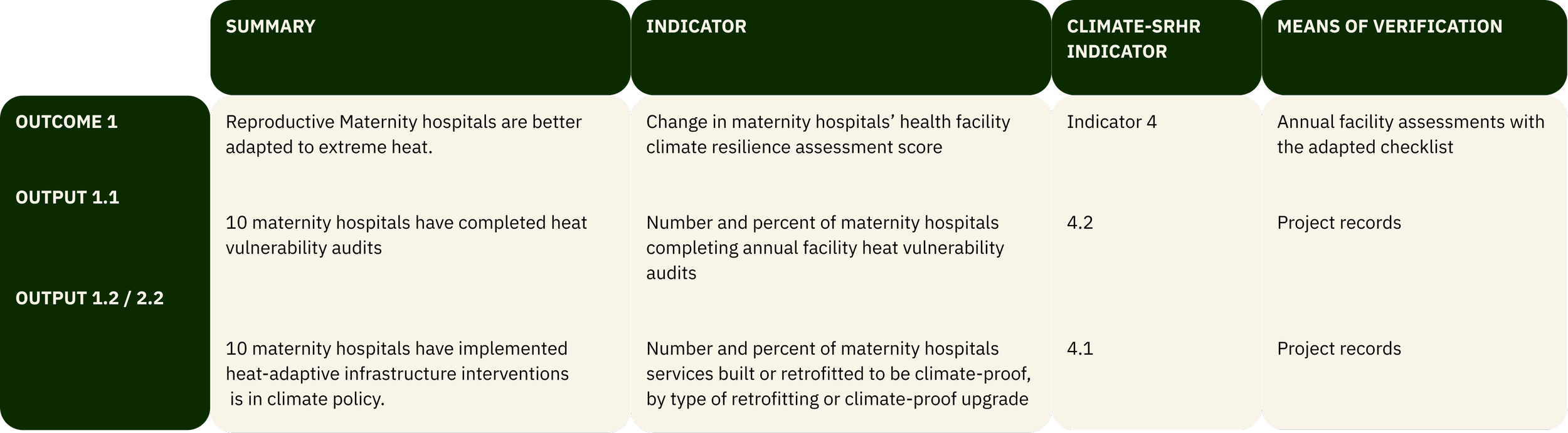
Using the MEL framework to select indicators
To select their indicators, the team reviewed the climate-SRHR indicator set to identify output, outcome, and impact indicators that aligned with their project’s activities. In some cases, they adapted the indicator slightly to reflect their specific program needs. For example, if an indicator referred to “climate and SRHR” generally, they instead adapted the indicator to focus on “extreme heat and pregnancy.” Once the indicators were selected, they reviewed any facility-dependent indicators with participating maternity hospitals to ensure feasibility.
Outcome 1: Maternity hospitals are better adapted to extreme heat.
The first outcome that this project aims to achieve is for maternity hospitals to be better adapted to extreme heat. This falls under Indicator 4: SRH service delivery points are prepared for climate hazards. For this project, this means they will be looking at the change in maternity hospitals’ health facility climate resilience assessment score. The team decided to adapt the WHO Checklists to Assess Vulnerabilities in Health Care Facilities in the Context of Climate Change by focusing specifically on heat-related risks and integrating a gender lens.
Outcome 2: Pregnant women are less exposed to extreme heat.
The second outcome that this project aims to achieve is for pregnant women to be less exposed to extreme heat. This falls under Indicator 10: Climate-SRHR action contributes to greater climate resilience beyond the health sector. For this project, this means they will be looking at the change in pregnant women's resilience to climate change, as measured by change in their exposure to extreme heat.
In addition to measuring exposure to high temperatures within maternity hospitals, the team also decided to monitor overall extreme heat days in the region as a contextual indicator. The team read a scoping review that discussed the different heat indices that are used to measure the effects of extreme heat on maternal health (Brimicombe et al. 2024). However, their technical capacity is fairly limited, as are local meteorological records. Therefore, the team decided to track these outcomes by installing temperature dataloggers indoors within maternity wards and outdoors at maternity hospitals. They will track the average temperature indoors and the number of days where the temperature exceeded 35C.
For more on defining and measuring extreme heat events, visit What are extreme climate and weather events, and how should we measure and define them?
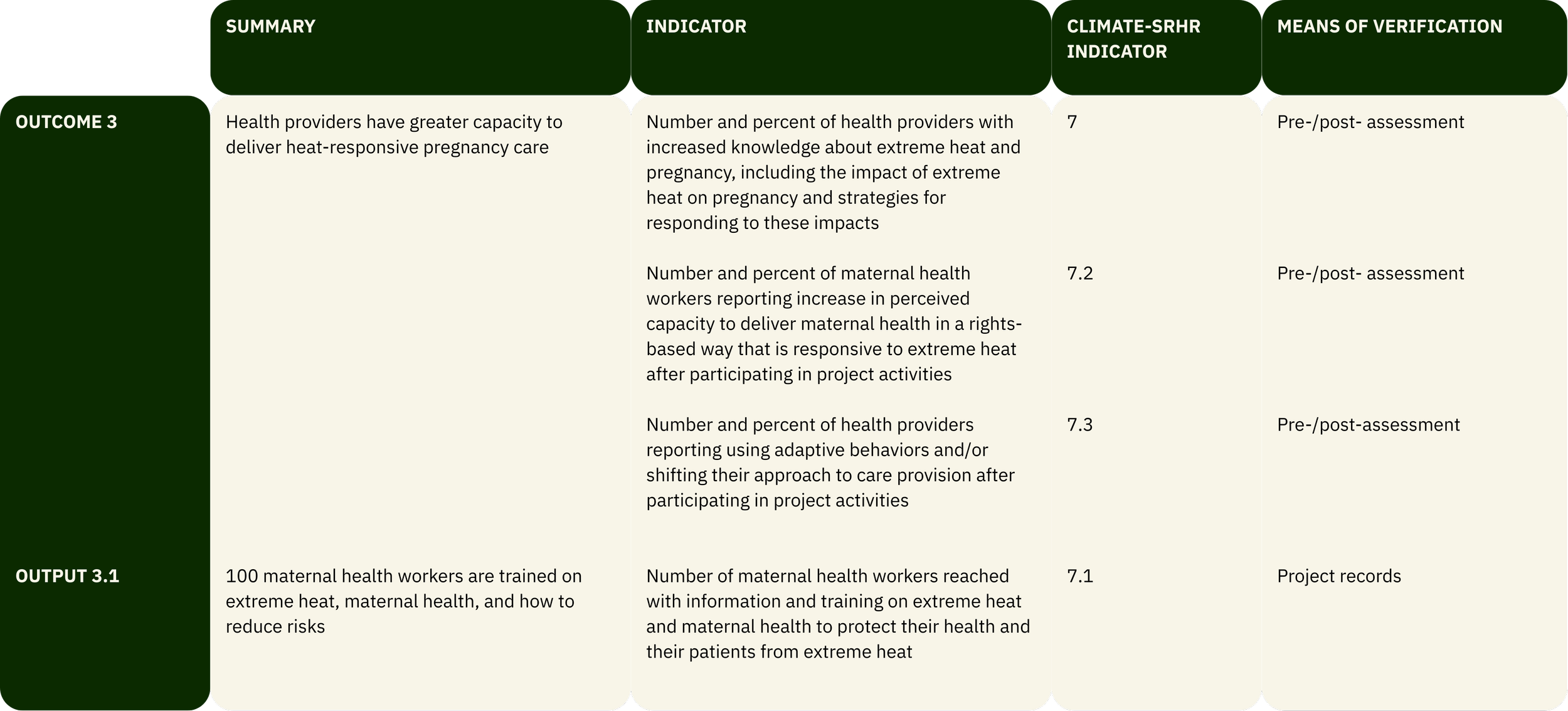
Outcome 3: Health providers have greater capacity to deliver heat-responsive pregnancy care.
The third outcome that this project aims to achieve is for health providers to have greater capacity to deliver heat-responsive pregnancy care. This falls under Indicator 7: The health workforce has the knowledge and skills to deliver climate-responsive SRH services. For this project, this means they will be looking at the change in pregnant women's resilience to climate change, as measured by change in their exposure to extreme heat.

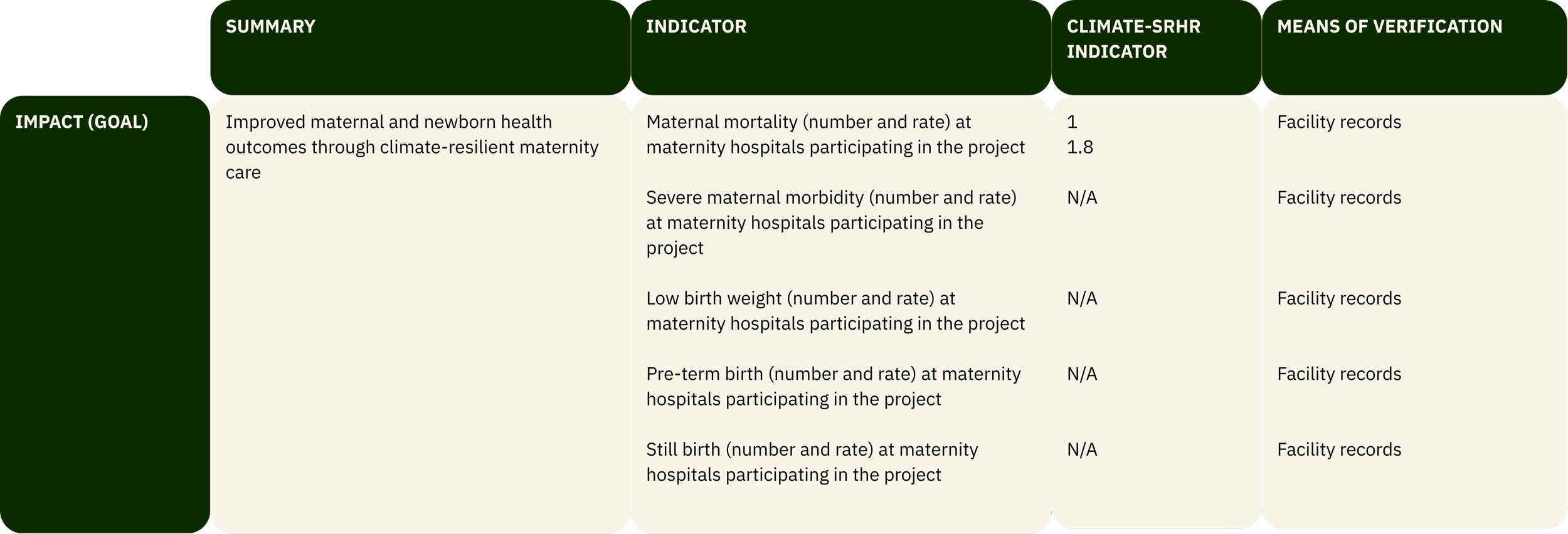
Impact: Improved maternal and newborn health outcomes through climate-resilient maternity care.
The overarching aim that this project will contribute to is improved maternal and newborn health outcomes through climate-resilient maternity care. This falls under Indicator 1: Climate-SRHR projects contribute to improved SRHR outcomes. For this project, this means that they will be looking at the change in heat-related maternal health outcomes at maternity hospitals participating in the project. After reviewing the Indicator 1 sub-indicators for maternal health, they select Indicator 1.8: Maternal mortality rate in climate-vulnerable areas benefiting from climate-responsive SRHR activities.
After coordinating with the maternity hospitals who would benefit from the project to identify what maternal and neonatal health outcomes would be feasible to track, the team decides to also track the number of maternal deaths at each participating facility, the number of cases of severe maternal morbidity, the number and percent of low birthweight babies, the number and percent of pre-term births, the number of stillbirths.
Implementing the MEL plan
The project team decided to assign a dedicated local staff manager to MEL for this project. That person’s responsibilities include data collection, data management, organizing learning sessions, and leading on reporting to the donor. They will be supported by data collectors and other project staff. Close coordination with the project manager will allow for continuous learning and rapid response during periods of extreme heat. Their MEL plan involves:
Monthly reporting from facility records
Post-training follow-ups will take place 3 and 6 months after training
Quarterly learning sessions with project staff, maternity hospital facility managers, and other key stakeholders
Annual focus group discussions and interviews with maternity hospital staff, cooling center visitors, and maternity hospital clients to provide additional verification and contextualization
Annual report to the donor
Project results and lessons learned shared with participating maternity hospitals, local and national government officials, and the global community at a conference
Learn from Others
This is a fictional case study, but across the globe, organizations are taking action to address extreme heat risks to SRHR:
The Women's Climate Shock Insurance and Livelihoods Initiative (WCS) - featured in one of our Climate-SRHR Evidence Hub Case Studies - provides extreme heat insurance, early warnings, and protective equipment to women in India affected by extreme heat.
The Climate, Heat and Maternal and Newborn Health in Africa (CHAMNHA) project aimed to reduce the effects of extreme heat on pregnant women. In Burkina Faso, the team conducted a series of community engagement and co-design activities to develop interventions. A similar co-design approach was also used in Kenya, where women who participated in the intervention reported an increase in understanding of heat risks during pregnancy and an increase in familial support with household tasks.
A team of researchers conducted a policy analysis of heat health action plans, examining how these plans incorporated pregnant women.